Diseases & Conditions
Neuromuscular Scoliosis
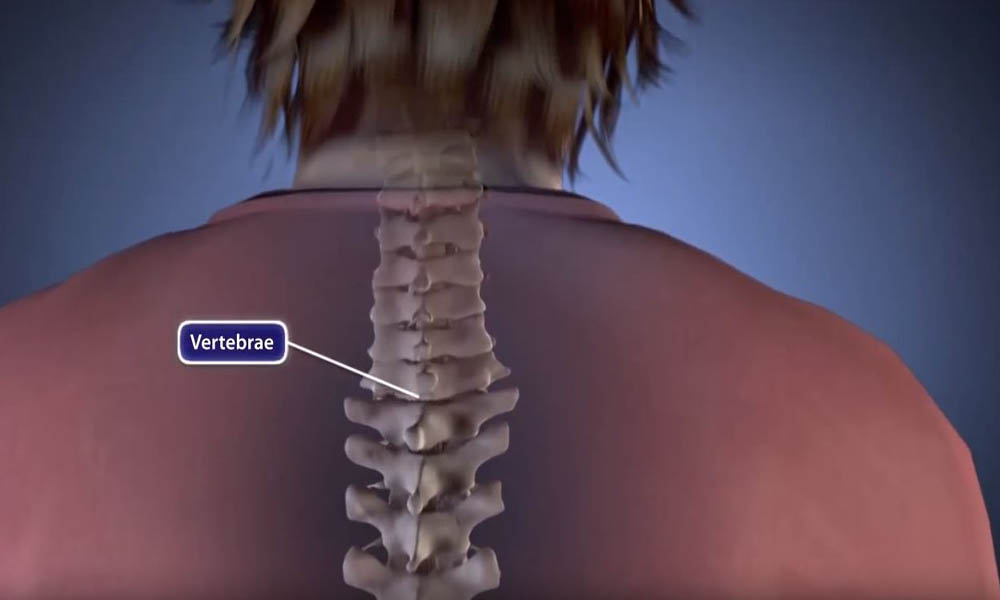
Scoliosis is a condition that causes the spine to curve sideways. Neuromuscular scoliosis (NMS) is a type of scoliosis that can occur in children who have medical conditions that impair their ability to control the muscles that support the spine. Common medical conditions associated with NMS include muscular dystrophy, cerebral palsy, and spina bifida.
Anatomy
Scoliosis causes the small bones of the spine to tilt and/or rotate so that instead of a straight line down the middle of the back, the spine looks more like the letter "C" or "S."
Because children with NMS can have a range of medical issues in addition to the spinal curve, treatment involves a team of doctors and health professionals from different medical specialties working together to provide care. In many cases of NMS, surgery is needed to correct the curvature and stabilize the spine.
Description
NMS is just one type of scoliosis that can affect children and adolescents. The other main types include:
- Idiopathic scoliosis. This is the most common type of scoliosis and often shows up in children when they reach puberty. Idiopathic means that the exact cause of the condition is not known.
- Congenital scoliosis. This type of scoliosis develops before birth. Babies with congenital scoliosis may have spinal bones that are not fully formed or are fused together.
In all types of scoliosis, spinal curves often become larger and more noticeable during periods of rapid growth, such as adolescence. Idiopathic and congenital scoliosis curves typically affect limited sections of the spine and stop progressing when an adolescent is full-grown. In contrast, NMS spinal curves often develop at a younger age than idiopathic scoliosis. These curves typically are long and involve the entire spine. In addition, NMS curves progress more rapidly and may continue to worsen even into adulthood.
Cause
NMS is caused by an underlying medical condition that affects the body's neurological system or muscular system — or a combination of both.
Although not all children with neuromuscular conditions develop NMS, it is common in children who use wheelchairs. With some neuromuscular conditions, a child may be able to walk when younger but may need to use a wheelchair when they reach adolescence. Because adolescence often coincides with a major growth spurt, this is a time when these children are at greatest risk for developing NMS or for having an existing curve progress.
The likelihood that a child will develop NMS is related to the extent of nerve and muscle involvement associated with their neuromuscular condition. The table below shows how the incidence of scoliosis increases according to the neuromuscular involvement of the underlying condition.
| Neuromuscular Condition | Incidence of Scoliosis |
|---|---|
| Cerebral palsy (2 limbs involved) | 25% |
| Myelodysplasia (lower lumbar) | 60% |
| Spinal muscle atrophy | 67% |
| Friedreich ataxia | 80% |
| Cerebral palsy (4 limbs involved) | 80% |
| Duchenne muscular dystrophy | 90% |
| Myelodysplasia (thoracic level) | 100% |
| Traumatic paralysis (<10 years) | 100% |
Source: Scoliosis Research Society
Symptoms
Signs of NMS in children who are able to walk are similar to those of children with idiopathic scoliosis:
- Tilted, uneven shoulders, with one shoulder blade protruding more than the other
- Prominent ribs on one side
- Uneven waistline
- One hip higher than the other
For children who use wheelchairs, spinal curves may cause changes in appearance like those described above, as well as changes that can hinder their performance of daily functions:
- Slouching or leaning more to one side
- Tilted pelvis
- A deteriorating ability to sit and the need to use the hands and arms for seating support
- Pressure sores that develop due to the pelvic tilt and overall imbalance
These changes can further impede a child's independence, making daily activities such as dressing and eating more difficult.
In addition, children with NMS may have other types of spinal curves, such as kyphosis (hunchback) or lordosis (swayback). Larger scoliosis curves in the upper back or hyperlordotic curves (excessive swayback) may reduce the space in the chest for the lungs and cause breathing problems.
Doctor Examination
Physical Examination
Before the physical examination, your child's doctor will discuss your child's family and medical histories and overall health, including which symptoms are present and when they began.
During the physical exam, your doctor will closely examine your child's back and spine. In addition, they will assess any problems with sitting balance, skin breakdown, or daily function.
Imaging Tests
Imaging tests help doctors assess the severity of your child's NMS.
X-rays. X-rays provide clear images of dense structures such as bone. An X-ray will allow your child's doctor to see the location of the curve on the spine and to measure the degree of the curvature.
Magnetic resonance imaging (MRI) scans. An MRI scan provides clear images of soft tissues and helps your child's doctor evaluate the health of the spinal cord.
Treatment
A multidisciplinary approach is needed to treat neuromuscular scoliosis. The treatment team may include specialists in orthopaedics, pediatrics, pulmonology, neurology, urology, nutrition, and gastroenterology. Coordination of care is very important and will help ensure that every aspect of treatment is maximized. In many cases, the NMS treatment team is led by the child's developmental pediatrician.
Treatment for NMS will depend on your child's age and underlying condition, as well as the type and severity of the spinal curve.
Nonsurgical Treatment
Although nonsurgical treatments will not prevent your child's curve from progressing, they may delay the progression and help improve function and quality of life. Nonsurgical treatments include:
Wheelchair modification. This is the most commonly recommended nonsurgical treatment. If your child has a shifted pelvis that affects balance, their wheelchair can be modified to improve posture. Modifications may include custom-molded chair backings and adjustment of the side positioners to help improve balance while sitting.
Bracing. For some patients in wheelchairs, the treatment team may recommend wearing a molded plastic brace around the upper body. This may provide a more stable sitting position and allow for use of the arms and hands. However, bracing will not prevent the progression of NMS curves, as it can in idiopathic scoliosis, and is not definitive treatment for NMS.
For NMS patients who are able to walk, wearing a brace may make them more likely to fall or lose their balance while walking — especially if they have significant muscle weakness, lung problems, or an unsteady gait.
Physical therapy. Specific exercises may help address your child's muscular imbalances and improve physical functioning.
Surgical Treatment
Indications for surgery. Your child's treatment team will consider several things when determining whether to recommend surgery to control the spinal curve, including how severe the curve is and how much it affects your child's function. The most common indications for surgery include:
- Curves greater than 50 degrees (in patients who are still growing)
- Curves greater than 50 degrees that have progressed more than 10 degrees (in patients who have reached skeletal maturity)
- Difficulty sitting and functional deterioration
- Pain
- Problems with heart or lung function
The decision to proceed with surgery in patients who cannot communicate is often very difficult and relies on the size of the spinal curve, the impact of the curve on sitting balance, and the care of the patient. Input from the family and/or caregiver is critical in this decision-making process.
Because NMS results from an underlying neuromuscular condition, the underlying condition guides the treatment strategy. For example, surgical decompression — a surgery that involves removing bone that may be compressing structures within the spine — may prevent curve progression in patients with hydrosyringomyelia (a fluid sac within the spinal cord). Patients who undergo this procedure may not need spinal stabilization.
Surgical stabilization of the spine. The goals of this treatment are to:
- Stabilize the curve and stop its progression
- Balance the spine and pelvis, thereby increasing sitting tolerance if the patient is in a wheelchair or improving walking if the patient can walk
- Improve lung function
- Reduce pain
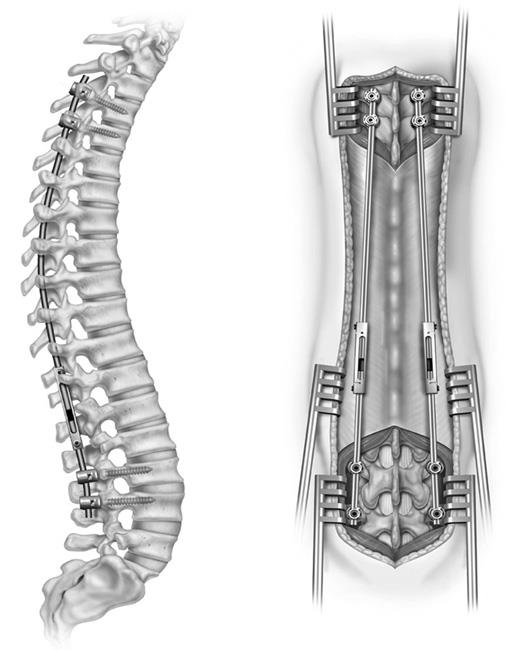
Growing Rods. Most operations to stabilize the spine also stop growth in the segment of the spine that is operated on. Temporary spinal stabilization with growing rods may be necessary in young children to allow the spine, chest, and lungs to grow as much as possible. The goal of a growing rod is to allow continued growth while correcting the curve and improving daily function.
During the procedure, the doctor attaches one or two rods to the spine above and below the curve. Every 6 to 8 months, the child returns to the doctor for a minor procedure to lengthen the rod(s) to keep up with the child's growth. When the child is fully grown, the doctor replaces the rod(s) and performs a spinal fusion.
A newer alternative is to implant magnetically-powered rods (MAGEC) that can be lengthened in the doctor's office, eliminating the need for repeated invasive surgeries. Some patients with NMS may not be candidates for MAGEC rods because of other magnetically or electrically placed implants.
Spinal Fusion. Spinal fusion is the most common surgical procedure used to treat NMS.
During the procedure, the curved vertebrae are fused together so that they heal into a single, solid fusion (bone mass). This will stop the growth completely in the abnormal segment of the spine and prevent the curve from worsening in the future.
Spinal fusion involves placing small pieces of bone graft between the vertebrae to be fused in an effort to increase the likelihood of a successful fusion. These graft pieces are obtained from a bone bank or made from an artificial material. Over time, the bone grows together — similar to when a broken bone heals.
Metal rods are typically used to hold the spine in place until the fusion happens. The rods are attached to the spine by hooks, screws, and/or wires. Once the bone graft fuses with existing bone, the straightened spine does not move, and the curve will not progress.
In patients who are still very immature and growing rapidly, spinal fusion may require both an anterior (front) and posterior (back) approach. This two-sided approach can help to avoid crankshaft syndrome, a problem in which areas of the spine that are still growing continue to rotate, while the instrumented areas remain fixed.
Because patients in wheelchairs often also have a pelvic tilt, it is common for the fusion to extend from the upper thoracic spine down to the sacrum (base of the spine) and pelvis.
Complications
Because NMS is associated with other underlying neuromuscular disorders and because surgery for NMS typically involves more areas of the spine, the complication rate after surgery is higher than with some other types of scoliosis. Your child's doctor will talk with you about potential complications and the steps taken prior to surgery to prevent them. For example, your child's treatment team will work to maximize nutrition and heart and lung status prior to surgery to minimize the risk of infection and the prolonged need for being on the ventilator after surgery. Similarly, before surgery, the team will fully assess your child's skin in the region of the spine and pelvis to minimize the risk for infection.
Last Reviewed
September 2019
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.