Diseases & Conditions
Spinal Deformity in Children with Myelomeningocele
Myelomeningocele, or spina bifida cystica, is a birth defect that occurs in the early weeks of fetal development. It is the most common and most serious type of spina bifida, a neural tube defect that occurs in about 1,400 babies born each year, according to the Centers for Disease Control.
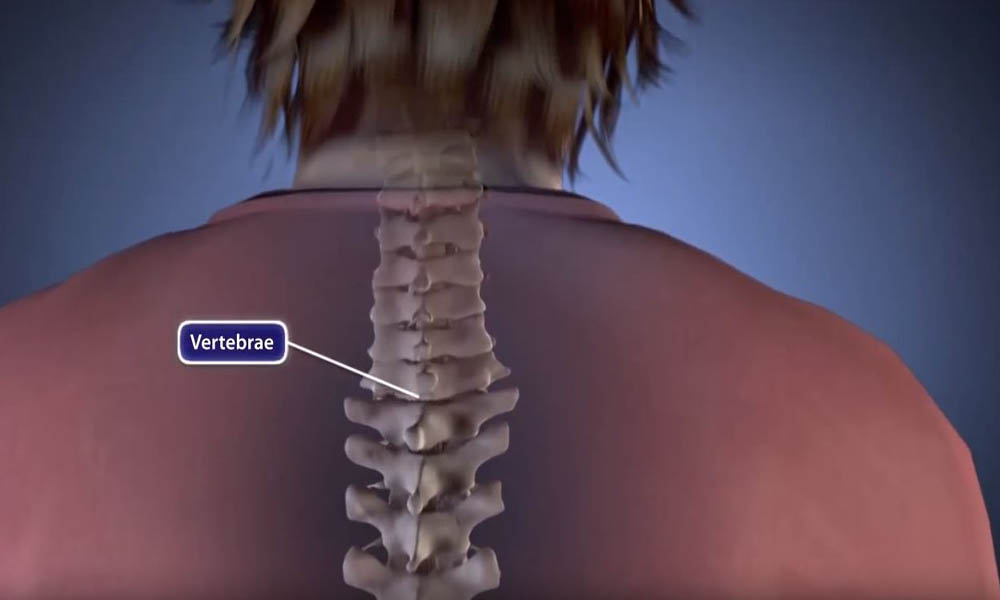
In babies with myelomeningocele, parts of some of the bones of the back (vertebrae) do not develop properly and do not close completely around the spinal cord. As a result, portions of the spinal cord, nerves, spinal fluid, and surrounding tissues push through the incomplete backbone and are exposed. These tissues often form a sac that sticks out of a baby's back.
The myelomeningocele opening or sac can form anywhere along the back, but it most often occurs in the lower back area. Infants typically lose nerve functioning below where the defect occurs in the spine. In many cases of myelomeningocele, infants and children have sensation loss, paralysis, and bowel and bladder problems. The paralysis can lead to deformities of the legs, feet, and back.
Many children with myelomeningocele develop severe deformities of the spine, such as scoliosis. This article focuses on the treatment of spinal deformities associated with myelomeningocele.
Because children with myelomeningocele can have a range of medical issues, treatment involves a team of doctors and health professionals from different medical specialties working together to provide care.
Cause
The cause of myelomeningocele is unknown.
It is known that taking folic acid reduces the risks for neural tube defects like spina bifida. Because these types of defects develop so early in pregnancy, doctors today advise prospective mothers to take folic acid prior to becoming pregnant, as well as during pregnancy. As a result, the incidence of neural tube defects like myelomeningocele is declining.
The development of a spinal problem, or curvature, is prevalent in the more severe cases of myelomeningocele. The curvature may be caused by:
- Weak trunk muscles that allow the spine to collapse (neuromuscular)
- Abnormally formed vertebrae (congenital)
- A combination of both
The three most common types of spinal deformity are:
- Scoliosis (sideways curvature of the spine to the left or right). Scoliosis in children with myelomeningocele most often results from a lack of neuromuscular control — weak trunk muscles that cannot support the spine. This kind of scoliosis may be associated with what is called tethering of the spinal cord.
- Kyphosis (exaggerated round back). Kyphosis can develop from muscle imbalances in a child's trunk that are associated with paralysis. A particularly severe form of this is called myelokyphosis, which is very stiff and can be associated with skin breakdown over the apex (highest point) of the prominence.
- Lordosis (exaggerated sway back). Lordosis can occur when a child's hip muscles are tight, causing the pelvis to push forward and an exaggerated swayback to develop.
Doctor Examination
A child with myelomeningocele requires the ongoing care of several medical specialists.
- An orthopaedic surgeon manages any bone or muscle problems that interfere with the child's ability to function
- A neurosurgeon monitors the health of the child's brain and spinal cord
- A urologist manages any bowel and bladder problems
- A physical rehabilitation doctor (physiatrist) helps customize braces and/or make any necessary wheelchair modifications
Treatment for a spinal curvature is led by a pediatric orthopaedic surgeon, but because these children have wide-ranging medical needs, the entire medical team must be involved to ensure the best outcome.
Physical Examination
Most children with myelomeningocele use wheelchairs due to partial or complete paralysis in their legs. A spinal curvature can cause sitting imbalances that put too much pressure on certain areas and result in skin problems. For example, the kyphosis prominence may press against the back of the wheelchair, causing pressure sores that become hard to heal.
A kyphosis curve may also force a child to lean forward and rely on their hands for constant support. Without the use of their hands, the child is not able to perform many daily activities.
The orthopaedic surgeon will examine the child's curvature and assess any problems with sitting balance, skin breakdown, or daily function.
Imaging Tests
X-rays. X-rays of the spine help the doctor evaluate the condition and position of the child's bones.
An X-ray will also show the doctor how severe the curve is. The doctor will measure the degree of the curve as it appears in the X-ray to determine the right treatment.
In general, curves measuring 20° or more are considered serious and require treatment. Curves greater than 45° to 50° will likely need surgery to restore a more normal posture.
Magnetic resonance imaging (MRI) scans. MRI scans provide clear images of soft tissues and help the doctor evaluate the health of the spinal cord.
Treatment
Many spinal deformities in children with myelomeningocele will worsen. As a spinal curvature progresses, risks for skin and functional problems increase. In addition, severe curves can collapse space in the chest, which can potentially cause heart and lung problems.
Nonsurgical Treatment
Bracing. If a child is still growing and the spine curvature is flexible, the doctor may recommend wearing a brace. Although bracing cannot straighten a spinal curve, it may slow down the curve progression and allow the child more growth before surgery is required.
Braces need to be custom-made so that they fit the child and do not cause any skin irritation or other problems.
Wheelchair modification. If a child has a shifted pelvis that affects balance, the wheelchair can be modified to improve posture. Like bracing, wheelchair modification can improve a child's function and slow the progression of a curve, but it should not be viewed as a cure.
Surgical Treatment
If bracing and/or wheelchair modifications are not effective at controlling the progression of spinal curve, or if a child comes to the doctor with a severe curvature of the spine, surgery may be necessary.
The operation for a spinal curve is a spinal fusion. The basic idea is to realign and fuse together the curved vertebrae so that they heal into a single, solid bone. Screws, rods, hooks, or wires will keep the bones in place. Spinal fusion can:
- Straighten the spine to improve posture and alleviate the need for the child to use their hands and arms to support their upper body
- Avoid pressure points from developing due to uneven sitting that can cause the skin to break down
The surgical treatment of children with spinal deformities associated with myelomeningocele can be difficult because of:
- An increased risk of surgical complications
- Additional medical problems, such as hydracephalus, skin conditions, and urinary tract infections
However, careful preoperative planning with a team of medical professionals, as well as new fusion implant designs, can result in successful outcomes.
Last Reviewed
April 2022
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.