Diseases & Conditions
Osgood-Schlatter Disease (Knee Pain)
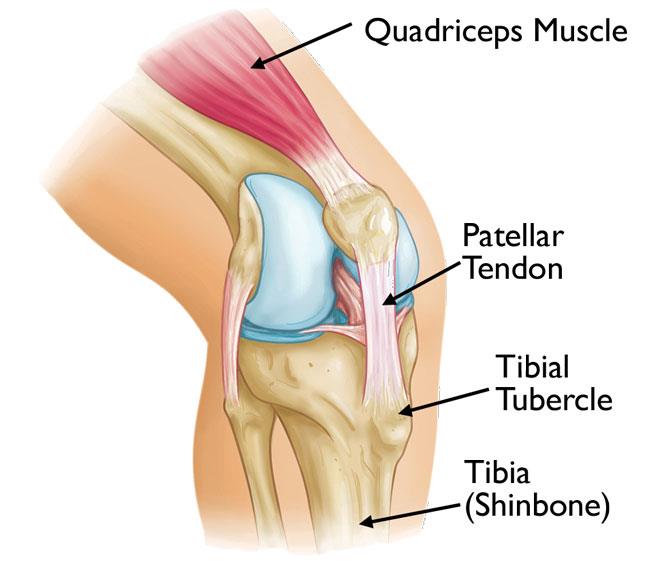
Osgood-Schlatter disease is a common cause of knee pain in growing adolescents. It is an irritation of the area just below the knee where the tendon from the kneecap (patellar tendon) attaches to the shinbone (tibia).
Osgood-Schlatter disease most often occurs during growth spurts, when bones, muscles, tendons, and other structures are changing rapidly. Because physical activity puts additional stress on bones and muscles, children who participate in athletics — especially running and jumping sports — are at an increased risk for this condition. However, less active adolescents may also experience this problem.
In most cases of Osgood-Schlatter disease, simple measures like rest, ice, over-the-counter pain medication, and stretching and strengthening exercises will relieve pain and allow a return to daily activities.
Description
The bones of children and adolescents have a special area where the bone is growing called the growth plate. Growth plates are areas of cartilage located near the ends of bones. When a child is fully grown, the growth plates harden into solid bone.
Some growth plates serve as attachment sites for tendons, the strong tissues that connect muscles to bones. A bony bump called the tibial tubercle covers the growth plate at the end of the tibia. The group of muscles in the front of the thigh (called the quadriceps) attaches to the tibial tubercle.
When a child is active, the quadriceps muscles pull on the patellar tendon which, in turn, pulls on the tibial tubercle. In some children, this repetitive traction (pulling) on the tubercle leads to irritation of the growth plate. The prominence, or bump, of the tibial tubercle may become very pronounced.
Symptoms
Painful symptoms are often brought on by running, jumping, and other sports-related activities. In some cases, both knees have symptoms, although one knee may be worse than the other. Symptoms include:
- Knee pain and tenderness at the tibial tubercle
- Swelling at the tibial tubercle
- Tight muscles in the front or back of the thigh
Doctor Examination
During the appointment, your child's doctor will:
- Discuss your child's symptoms and general health.
- Conduct a thorough examination of the knee to determine the cause of the pain. This will include applying pressure to the tibial tubercle, which should be tender or painful for a child with Osgood-Schlatter disease.
- Possibly ask your child to walk, run, jump, or kneel to see if the movements bring on painful symptoms.
The diagnosis of Osgood-Schlatter disease is made by the doctor based on history and physical exam. X-rays are not needed to make the diagnosis and should only be performed if the doctor has other concerns about your child's knee pain during the visit.
Treatment
Treatment for Osgood-Schlatter disease focuses on reducing pain and swelling.
In severe cases where your child is limping or having a large amount of pain even at rest, it may be necessary for your child to limit exercise activity for a short period of time while they begin a stretching and strengthening program.
The pain may continue at some level until the growth plate closes. The goal is to make the pain a dull ache that does not affect your child's ability to participate in sports activities and goes away quickly once the activity is over.
It is important to know that continued participation in activity will not cause long-term damage to the knee. It is safe for children to participate in activities as tolerated.
However, if the pain starts to make the activity not fun anymore, or your child is considering not participating due to pain and is already doing all of the treatment methods listed below, they should see their doctor to discuss activity modification and other newer treatments.
Your child's doctor may recommend additional treatment methods, including:
- Stretching exercises. Stretches for the front and back of the thigh (quadriceps and hamstring muscles) may help relieve pain and prevent the disease from returning. These should be performed 3 to 4 times per day.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Drugs like ibuprofen or naproxen reduce pain and swelling.
- Ice. Icing the inflamed area may reduce pain and swelling. Use cold packs for 20 minutes at a time, several times a day, especially after physical activity. Do not apply ice directly to the skin.
- Patellar tendon strap. This is a band that is worn around the upper part of the leg over the middle of the patellar tendon, just between the bottom of the kneecap and the bump on the tibial tubercle.
Outcome
Most symptoms will completely disappear when a child completes the adolescent growth spurt, around age 14 for girls and age 16 for boys. For this reason, surgery is rarely recommended.
However, the prominence of the tubercle will persist (still be there) and may increase in size until the child is finished growing.
Last Reviewed
September 2024
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.