Treatment
Revision Total Hip Replacement
Total hip replacement is one of the most successful procedures in all of medicine. In the vast majority of cases, total hip replacement enables people to live more active lives without debilitating hip pain. Over time, however, a hip replacement can fail for a variety of reasons.
When this occurs, your doctor may recommend that you have a second operation to remove some or all of the parts of the original prosthesis and replace them with new ones. This procedure is called revision total hip replacement.
Although both procedures have the same goals—to relieve pain and improve function and quality of life—revision surgery is different than primary total hip replacement. Revision hip replacement is a longer, more complex procedure. It requires extensive planning, as well as the use of specialized implants and tools, in order to achieve a good result.
Description
During primary total hip replacement surgery, the hip joint is replaced with an implant or prosthesis made of metal, plastic, and/or ceramic components. Although most total hip replacements are very successful, problems can develop over time. These problems may require a revision procedure to replace the original components.
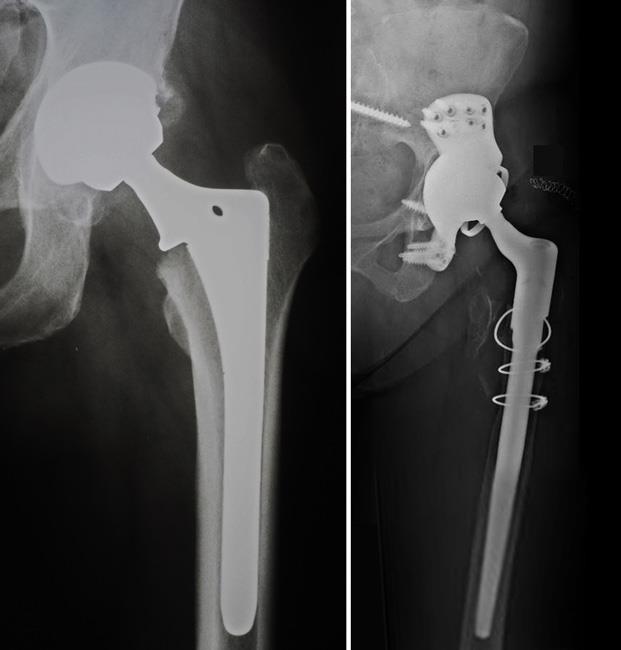
There are different types of revision surgery. In some cases, only some components of the prosthesis need to be revised. In other cases, the whole prosthesis needs to be removed or replaced and the bone around the hip needs to be rebuilt with augments (metal pieces that substitute for missing bone) or bone graft.
Damage to bone and soft tissue around the hip may make it difficult for the doctor to use standard primary hip implants for revision hip replacement. In most revisions, the doctor will use specialized implants that are designed to compensate for the damaged bone and soft tissue.
When Revision Total Hip Replacement Is Recommended
Implant Wear and Loosening
In order for a total hip replacement to function properly, an implant must remain firmly attached to the bone. During the initial surgery, the hip replacement components were either cemented into place or were "press fit" into the bone to allow bone to grow onto them. Sometimes, however, bone may fail to grow onto press-fit components. In addition, cemented or press-fit components that were once firmly fixed to the bone can eventually loosen, resulting in a painful hip.
The cause of loosening is not always clear, but repetitive high-impact activities, excessive body weight, and wear of the plastic liner between the ball and the metal cup are all factors that may contribute.
In addition, patients who are younger when they undergo the initial hip replacement may "outlive" the life expectancy of their artificial hip. For these patients, there is a higher long-term risk that revision surgery will be needed due to loosening or wear.
In some cases, tiny particles that wear off the cup's plastic liner accumulate around the hip joint and are attacked by the body's immune system. This immune response also attacks the healthy bone around the implant, leading to a condition called osteolysis In osteolysis, the bone around the implant deteriorates, making the implant loose or unstable.
Fortunately, plastics have improved greatly over the years, so plastic wear and osteolysis occur less frequently today than they did with earlier generations of implants.
Infection
Infection is a potential complication of any surgical procedure, including total hip replacement. Infection occurs when bacteria attach in and around the surface of the prosthesis. Infection may occur while you are in the hospital or after you go home. It may even occur years later.
If a total hip replacement becomes infected, it can be painful and the implant may begin to lose its attachment to the bone. Even if the implant remains properly fixed to the bone, there may still be pain, instability, and drainage from the infection. Because bacteria cannot be easily eliminated from a joint replacement with antibiotics alone, revision surgery is usually necessary.
Revision surgery for infection can be done in different ways. To determine which procedure is best for you, your doctor will consider a number of factors, including:
- The type of bacteria
- The duration and severity of the infection
- Your preference for a specific treatment
Debridement. In this procedure, your doctor will open up your hip, wash out the bacteria, and exchange the ball and plastic liner. The metal implants that are firmly attached to the bone are left in place. After debridement, you will receive intravenous antibiotics for several weeks to help cure the infection.
Staged surgery. In some cases, the implants must be completely removed. If the implants are removed to treat the infection, your doctor will usually perform the revision in two separate surgeries.
In the first surgery, your doctor will remove the implants and place a temporary cement spacer in your hip. This spacer is treated with antibiotics to help fight the infection and will remain in your hip for several weeks. During this time, you will also receive intravenous antibiotics.
When the infection has been cleared, your doctor will perform a second surgery to remove the antibiotic spacer and insert a new prosthesis. In general, removing the implant leads to a higher chance of curing the infection, but is associated with a longer recovery.
In some cases, your doctor may be able to remove the implants, wash out the hip, and place a new prosthesis all in the same operation. This procedure, which is called a one-stage exchange, may be appropriate in limited situations.
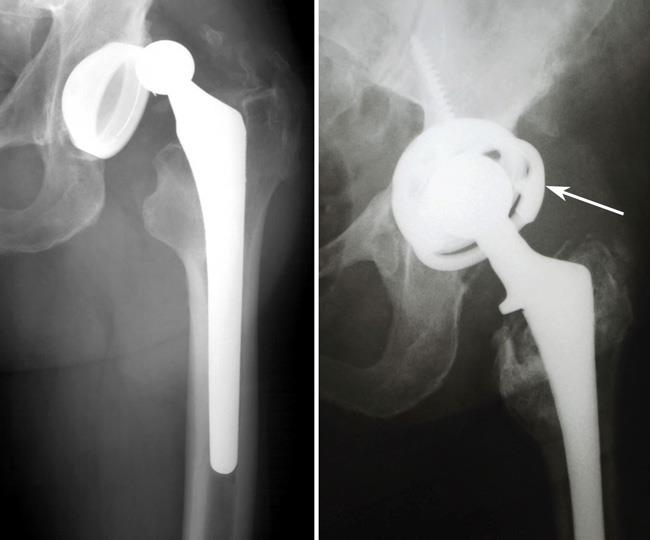
Recurrent Dislocation
A hip replacement has a ball-and-socket structure like that of your natural hip. For a hip replacement to work well, the ball must remain inside the socket. Trauma or certain hip positions can sometimes cause the ball to become dislodged from the socket. This is called a "hip dislocation." If you experience recurrent hip dislocations, you may need revision surgery to better align your hip joint or to insert a special implant designed to prevent dislocations.
Fracture
A periprosthetic fracture is a broken bone that occurs around the components of an implant. These fractures are most often the result of a fall, and often require revision surgery. To determine whether a revision is needed, your doctor will consider several factors, including the amount of remaining bone, whether your implant is loose, and the location of the fracture.
In rare circumstances, an implant itself can break. This also requires revision surgery.
Reaction to Metal Ions and Allergy to Metal
Over time, the metals used in implants can break down or wear, causing tiny particles to fall off the device into the space around the implant. This is more common with "metal-on-metal" devices, in which both the ball and socket components are made of metal. In some patients, sensitivity to the metal ions in these particles can result in damage to the bone and soft tissues around the hip and lead to the need for revision surgery.
In very rare cases, a patient allergy to the metal used in implants may cause pain around the site of the implant. There is no definitive agreement among doctors regarding metal allergy in this setting, however, and more studies are needed.
Other Factors
The likelihood of needing revision hip replacement is also impacted by individual differences among patients. For example, patients who are younger and more active are more likely to experience issues related to implant wear. Patients who have certain medical conditions, such as obesity or diabetes, and those who have had certain surgical procedures in the past, are more likely to experience infection or implant failure.
Preparing for Surgery
Medical Evaluation
You will be asked to schedule a complete physical examination with your primary care doctor several weeks before revision surgery. This is to ensure that you are healthy enough to have the surgery and complete the recovery process. Patients who have chronic medical conditions, such as heart disease, may also be evaluated by a specialist, such as a cardiologist, before surgery.
Tests
Imaging tests. Your doctor will usually order imaging tests to learn more about the condition of your hip. This may include:
- X-rays: X-rays provide images of dense structures, such as bone. Your doctor may order x-rays of the joint replacement to look for loosening or a change in the position of the components.
- Other imaging tests. A nuclear medicine bone scan may help determine if the prosthesis has loosened from the bone. In some cases, a magnetic resonance imaging (MRI) scan or a computerized tomography (CT) scan will be used to help determine why your hip has failed and the condition of the bone.
Laboratory tests. Your doctor may order blood tests to help determine if you have an infection or are having a reaction to the metal components in your hip. Your doctor may also aspirate your hip. In this procedure, joint fluid is removed using a needle and syringe and then analyzed in a laboratory to determine if infection is present.
Home Planning
Because your mobility will be limited after surgery, you may need help for several weeks with such tasks as cooking, shopping, bathing, and doing laundry if you live alone.
Your doctor's office, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at home. Depending on your condition, you may need to stay at a nursing facility or rehabilitation center for some time after you leave the hospital. Your healthcare team can also help you arrange for a short stay in an extended care facility during your recovery if necessary.
Surgical Procedure
You will most likely be admitted to the hospital on the day of surgery.
Anesthesia
After admission, you will be evaluated by a member of the anesthesia team. The most common types of anesthesia used are general anesthesia (you are put to sleep) and spinal, epidural, or regional nerve block anesthesia (you are awake, but your body is numb from the waist down). The team, with your input, will determine which type of anesthesia will be best for you.
Procedure
Revision total hip replacement is a more complex procedure and takes longer to perform than primary total hip replacement. In most cases, the surgery takes several hours.
To begin, your doctor will follow the line of the incision made during your primary total hip replacement. The incision may be extended, however, to allow the old components to be removed. Once the incision is made, your doctor will expose the hip joint.
After exposing the joint, your doctor will examine the soft tissues in your hip to make sure that they are free from infection and other problems, such as a reaction to the metal components. He or she will assess all parts of the prosthesis to determine which ones have become worn or loose or shifted out of position.
Your doctor will then remove the original implant very carefully to preserve as much bone as possible. If cement was used in the primary total hip replacement, this is removed, as well. Removing this cement from the bone is a time-consuming process that adds to the complexity and length of the revision surgery.
Occasionally, a controlled "fracture" of the femur (thighbone) will be performed in order to remove a well-fixed stem. The femur will be put back together once the new stem is in place.
After removing the original implants, your doctor will prepare the bone surfaces in the pelvis and the femur for the revision implants. In some cases, there may be significant bone loss in these areas. If this occurs, metal augments or bone graft can be added to make up for the bony deficits.
Finally, your doctor will insert the specialized revision implants. Often multiple screws are required to hold the new cup in place until bone grows in. Your doctor will test the motion of the joint to ensure the implants are well-fixed and that the ball is stable inside the socket.
Special "trial" implants are usually tested prior to inserting and fixing the final components. A drain may be placed in your hip to collect fluid or blood that may remain after surgery.
After surgery, you will be moved to the recovery room, where you will remain for several hours while your recovery from anesthesia is monitored. When you wake up, you will be taken to your hospital room.
Complications
As with any surgical procedure, there are risks associated with revision total hip replacement. Because the procedure is longer and more complex than primary total hip replacement, it has a greater risk of complications. Before your surgery, your doctor will discuss each of the risks with you and will take specific measures to help avoid potential complications.
The possible risks and complications of revision surgery include:
- Dislocation
- Infection
- Blood clots
- Pulmonary embolism—a blood clot in the lungs
- Leg-length inequality
- Heterotopic ossification—new bone may form where it is not normally present
- Fracture
- Damage to nerves or blood vessels
- Failure of the bone to attach to the metal implant
- Implant loosening
Your Recovery in the Hospital
You will most likely stay in the hospital for several days. Although recovery after revision is usually slower than recovery after primary hip replacement, the type of care you will receive is very similar.
Pain Management
After surgery, you will feel some pain. Your doctor and nurses will work to reduce your pain, which can help you recover from your surgery faster.
Many types of medicines are available to help manage pain, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Opioids can provide excellent pain relief, however, they are narcotics and can be addictive. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Physical Therapy
Specific exercises will help strengthen your leg and restore function so that you may begin walking and resume your other daily activities as soon as possible after surgery. You may have weight-bearing limitations at first, depending on the complexity of your surgery. You may also be given certain hip precautions (positions to avoid) in order to prevent dislocation.
Blood Clot Prevention
Your doctor may prescribe one or more measures to prevent blood clots and decrease leg swelling. These may include special graded compression stockings, inflatable leg coverings (compression boots), and blood thinners.
Foot and ankle movement will be encouraged immediately following surgery. This is done to increase blood flow in your leg muscles to help prevent leg swelling and blood clots.
Preventing Infection
One of the most serious complications facing patients who undergo revision surgery is infection. Although infection occurs in only a small percentage of patients, it can prolong or limit full recovery. To prevent infection, you will be given antibiotics both before and after surgery. The risk of infection is slightly higher after revision surgery than after primary total hip replacement.
Your Recovery at Home
You will need some help at home for several days to several weeks after discharge. Before your surgery, arrange for a friend, family member or caregiver to provide help at home. You may need a walker, cane, or crutches for the first few days or weeks until you are comfortable enough to walk without assistance. If you are not allowed to put weight on your operative leg, you may need to use a walking aid for a longer period of time.
Wound Care
You may have stitches, staples, or glue running along your wound or sutures beneath your skin. The stitches or staples will be removed several weeks after surgery. Sutures beneath your skin will not require removal.
Avoid soaking the wound in water until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Physical Therapy
It is important to continue moving and exercising when you are home. Your physical therapist will provide you with specific exercises to help increase your strength and mobility and improve your ability to do everyday activities. Your therapist will also work with you to ensure that you understand and are following your hip precautions.
Preventing Complications
Follow your doctor's instructions carefully to reduce your risk of developing complications, including blood clots and infection, during the first several weeks of your recovery. He or she may recommend that you continue taking the blood-thinning and antibiotic medications that you started in the hospital.
Long-Term Outcomes
The vast majority of patients who undergo revision surgery experience favorable long-term outcomes. This includes relief from pain, increased stability, and better function. Complete pain relief and restoration of function are not always achievable, however, and some patients may still experience some pain or dysfunction following revision surgery.
Last Reviewed
April 2017
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.