Treatment
Robotic-Assisted Joint Replacement
This article focuses on robotic hip and knee replacement. Traditional hip and knee replacement are addressed in separate articles: Total Hip Replacement, Total Knee Replacement, Unicompartmental (Partial) Knee Replacement
Over the past decade, advances in imaging and instrumentation have led to the development of robotic-assisted surgery — an approach that helps surgeons plan and perform a variety of procedures with a high degree of accuracy. This includes total hip, total knee, and partial knee replacements.
With traditional hip and knee replacement procedures, the surgeon uses traditional cutting jigs (templates, or guides) and instruments to prepare the bone surfaces and align the joint.
Robotic-assisted joint replacements instead combines three-dimensional planning before surgery with real-time computer navigation during surgery. Using robotic tools that have sensory feedback, the surgeon can remove damaged bone and cartilage and implant artificial joints with greater precision, as well as help to preserve healthy tissue.
Your orthopaedic surgeon will discuss different surgical options with you and determine which approach will give you the best outcome.
Anatomy
Hip Joint
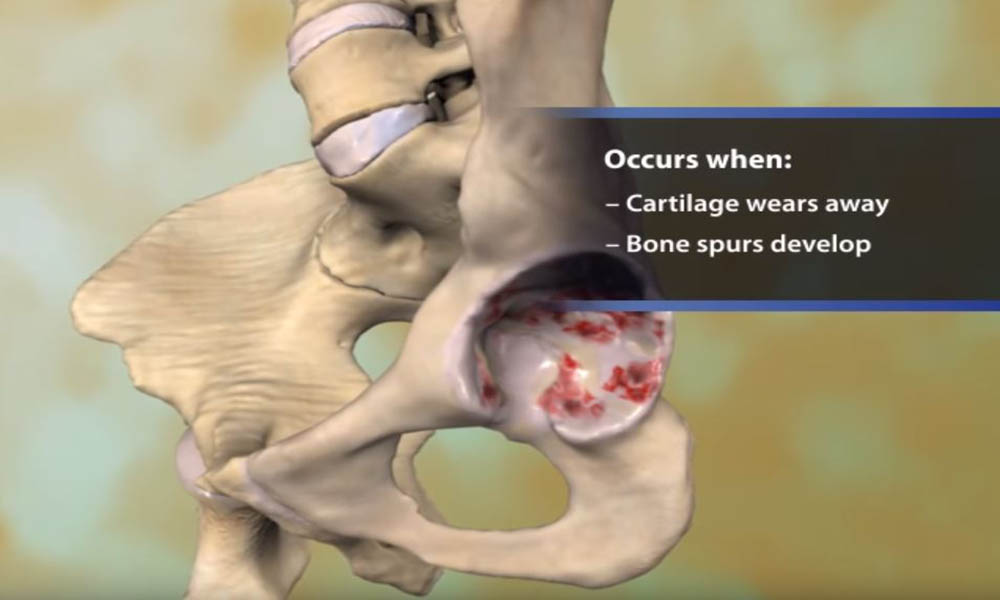
The hip is a ball-and-socket joint. The ball is the femoral head, which is the upper end of the femur (thighbone). The socket is the acetabulum, which is part of the pelvis bone.
The bone surfaces of the ball and socket are covered with articular cartilage. This is smooth tissue that cushions the ends of the bones and enables them to move easily.
A thin tissue called the synovial membrane surrounds the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates the cartilage. This eliminates almost all friction during hip movement.
Bands of tissue called ligaments (the hip capsule) connect the ball to the socket. This provides stability to the joint.
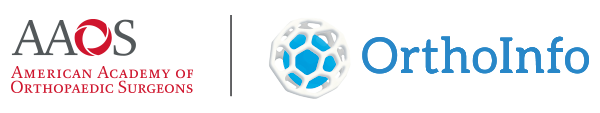
Knee Joint
The knee is a hinge joint made of the lower thighbone (femur), the upper shinbone (tibia), and the kneecap (patella). The ends of these bones are covered with articular cartilage, which is a smooth tissue that cushions the ends of the bones. This allows the joint to move easily.
The menisci are C-shaped structures located between the femur and tibia. They act as shock absorbers to cushion the joint.
Large ligaments (the cruciates and collaterals) hold the femur and tibia together and provide stability. The long thigh muscles (the quadriceps and hamstrings) give the knee strength.
A thin tissue called the synovial membrane surrounds the knee joint. In a healthy knee, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost all friction during knee movement.
Causes of Hip and Knee Pain
In hip and knee arthritis, the cartilage protecting the bones of the knee wears away. This can occur throughout the joint or just in a single area. Joint replacement is the surgical treatment for advanced arthritis.
There are several types of hip and knee arthritis:
- Osteoarthritis. This is an age-related, wear-and-tear type of arthritis. It usually occurs in people 50 years of age and older but may also occur in younger people. The cartilage that cushions the bones of the hip or knee softens and wears away. The bones then rub against one another, causing joint pain and stiffness.
- Rheumatoid arthritis. In this disease, the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed inflammatory arthritis.
- Posttraumatic arthritis. This can follow a serious hip or knee injury. Fractures of the bones surrounding the joint or tears of ligaments may damage the articular cartilage over time, causing joint pain and limiting joint function.
- Osteonecrosis. An injury to the hip or knee, such as a dislocation or fracture, may limit the blood supply to the bone. This is called osteonecrosis (also sometimes referred to as avascular necrosis). The lack of blood may cause the surface of the bone to collapse, and arthritis will result. Some diseases can also cause osteonecrosis.
- Childhood hip disease that leads to arthritis. Some infants and children have hip problems, such as abnormal development (dysplasia) of the hip. Even if the problems are successfully treated during childhood, they may still cause arthritis later in life. This happens because the hip may not grow normally, and the joint surfaces are affected.
Advantages and Disadvantages of Robotic-Assisted Joint Replacement
In both traditional and robotic-assisted joint replacement surgery, the damaged bone and cartilage are removed and replaced with prosthetic components.
- In total knee replacement, the equivalent of a prosthetic cap is placed on the ends of the bone.
- For a hip replacement, the entire joint is replaced with metal, ceramic, and plastic implants.
- Only the damaged compartment is replaced in a partial (unicompartmental) knee replacement surgery, while healthy cartilage and bone and all of the ligaments are preserved.
For a robotic procedure, special imaging is often obtained before surgery to create a customized 3-D plan for your joint replacement, depending on which robotic platform the surgeon uses.
Robotic-assisted total joint replacement surgery takes the same amount of time as a traditional joint replacement. And like traditional joint replacement, the procedure can be performed in a hospital operating room or an outpatient surgery center.
The potential advantages of robotic-assisted joint replacement surgery include:
- A joint replacement that is well-aligned and stable and that specifically minimizes the errors that can occur in patients who have unique variations in their joint anatomy
- More precise joint replacement in cases of challenging anatomy (like a stiff spine above a hip with arthritis or hip dysplasia)
- The ability to create a customized surgical plan and choose the ideal implant sizes before surgery
The disadvantages of robotic-assisted joint replacement surgery include:
- Possible need for additional imaging (CT scan) before surgery
- Possible risk of bone fractures where the navigation pins are placed
Your Surgery
During the surgery, your surgeon will place navigation pins into your bone to guide the robotic-assisted instruments in space. The robotic instruments provide sensory feedback to assist the surgeon in precisely removing damaged bone and cartilage and replacing it with prosthetic (artificial) components.
The prosthetic components mimic the shape and movement of the joint. These are made of a combination of metal, plastic, and ceramics.
After surgery, you will be taken to the recovery room, where you will be closely monitored by nurses as you recover from the anesthesia. You will then be taken to your hospital room, or discharged home if your procedure is being done on an outpatient basis.
Complications
Your doctor will explain the potential risks and complications of robotic-assisted joint replacement, including those related to the surgery itself and those that can occur over time after your surgery.
Most complications can be treated successfully. Some of the more common complications of joint replacement surgery include:
- Infection
- Blood clots
- Nerve injury
- Implant problems, like loosening or dislocation
Like traditional joint replacement surgery, robotic-assisted surgery should be performed by a well-trained, highly experienced orthopaedic surgeon. Your orthopaedic surgeon can talk to you about their experience with robotic-assisted joint replacement surgery, and the possible risks and benefits of the techniques for your individual treatment.
Recovery
Most patients go home 1 to 3 days after surgery. Many can even go home the same day as their procedure.
Weightbearing
You may put weight on your leg immediately after surgery, depending on your doctor's preferences and the strength of your bone. You may need a walker, cane, or crutches for the first few days or weeks until you are comfortable walking without assistance.
Pain Management
You can expect some pain and discomfort for several weeks after surgery. Your doctor may prescribe pain medicine, if needed. Treating pain with medications can help you feel more comfortable, which will help your body heal and recover from surgery faster.
Many types of pain medication are available to help control pain, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs) and local anesthetics. Opioids can provide excellent pain relief, but they are narcotics and can be addictive. It is important to take opioids only as directed by your doctor and to stop taking them as soon as your pain starts to improve.
Physical Therapy
Your doctor may recommend physical therapy after surgery. The physical therapist will give you exercises to help maintain your range of motion and restore your strength.
You will continue to see your orthopaedic surgeon for follow-up visits in their clinic at regular intervals.
You will most likely be able to resume your regular activities of daily living by about 6 to 12 weeks after surgery.
Last Reviewed
September 2022
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.