Treatment
Total Hip Replacement
Whether you have just begun exploring treatment options or have already decided to undergo total hip replacement surgery, this article will help you understand the benefits and limitations of total hip replacement. This article describes:
- How a normal hip works
- The causes of hip pain
- What to expect from total hip replacement surgery
- Which exercises and activities will help restore your mobility and strength, and enable you to return to everyday activities
If your hip has been damaged by arthritis, a fracture (a break in the bone), or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff, and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting.
If medications, changes in your everyday activities, and the use of walking supports do not adequately help your symptoms, you may consider total hip replacement surgery. Total hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
Total hip replacement surgery is one of the most successful operations in all of medicine. Since the early 1960s, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of total hip replacement. According to the Agency for Healthcare Research and Quality, more than 450,000 total hip replacements are performed each year in the U.S.
Anatomy
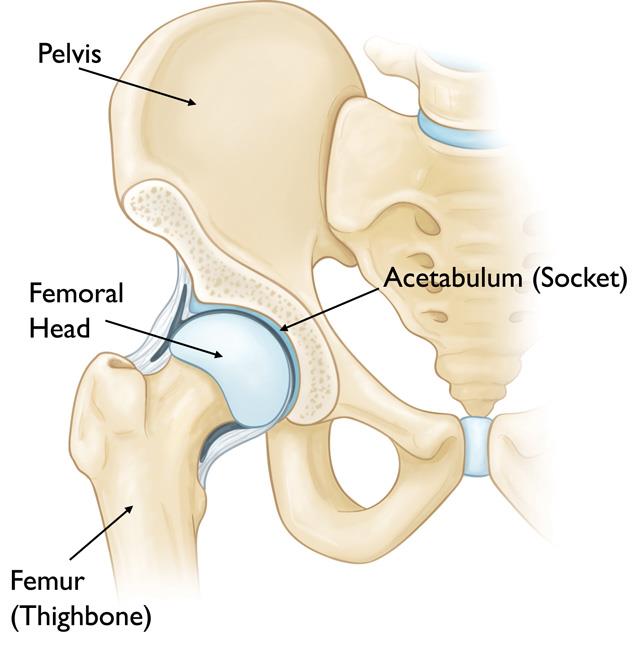
The hip is one of the body's largest joints. It is a ball-and-socket joint.
- The socket is formed by the acetabulum, which is part of the pelvis bone.
- The ball is the femoral head, which is the upper end of the femur (thighbone).
The bone surfaces of the ball and socket are covered with articular cartilage, a smooth tissue that cushions the ends of the bones and enables them to move easily.
A thin tissue called the synovial membrane surrounds the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost all friction during hip movement.
Bands of tissue called ligaments (the hip capsule) connect the ball to the socket and provide stability to the joint.
Common Causes of Hip Pain
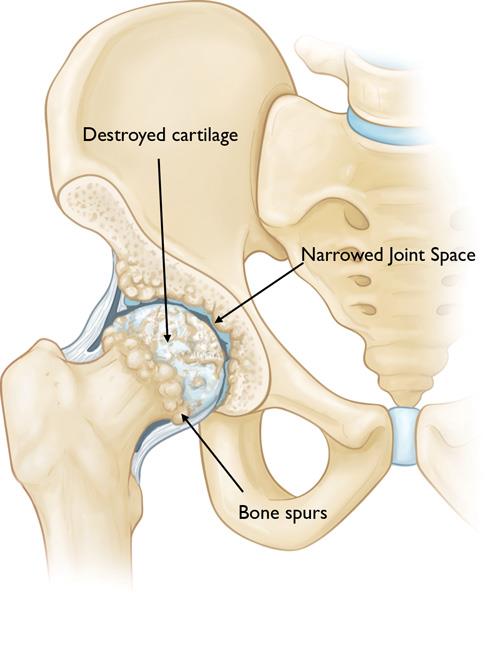
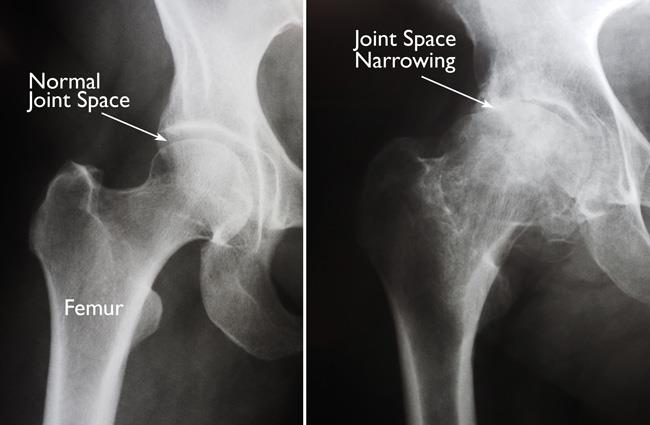
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis are the most common forms of this disease.
- Osteoarthritis. This is an age-related wear-and-tear type of arthritis. It usually occurs in people 50 years of age and older and often in individuals with a family history of arthritis. The cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness. Osteoarthritis may also be caused or accelerated by subtle irregularities in how the hip developed in childhood.
- Rheumatoid arthritis. This is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. This chronic inflammation can damage the cartilage, leading to pain and stiffness. Rheumatoid arthritis is the most common type of a group of disorders termed inflammatory arthritis.
- Posttraumatic arthritis. This can follow a serious hip injury or fracture. The cartilage may become damaged and lead to hip pain and stiffness over time.
- Osteonecrosis. An injury to the hip, such as a dislocation or fracture, may limit the blood supply to the femoral head. This is called osteonecrosis (also sometimes referred to as avascular necrosis). The lack of blood may cause the surface of the bone to collapse, and arthritis will result. Some diseases can also cause osteonecrosis.
- Childhood hip disease. Some infants and children have hip problems. Even though the problems are successfully treated during childhood, they may still cause arthritis later in life. This happens because the hip may not grow normally, and the joint surfaces are affected. Learn more: Developmental Dysplasia of the Hip (DDH), Adolescent Hip Dysplasia
Description
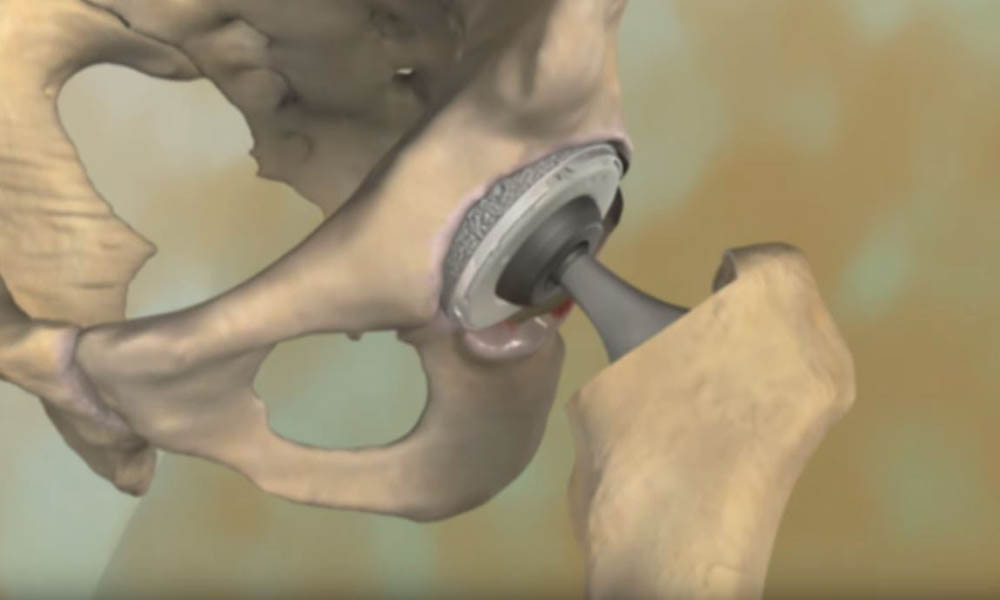
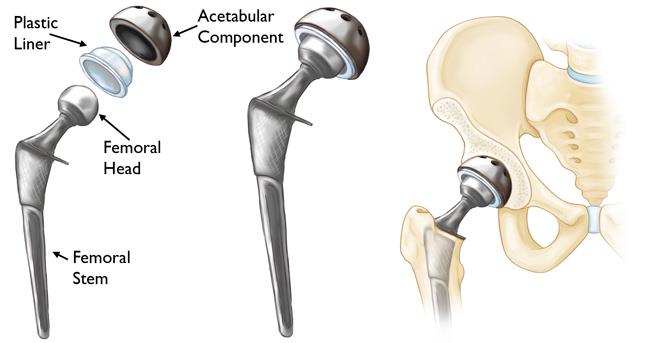
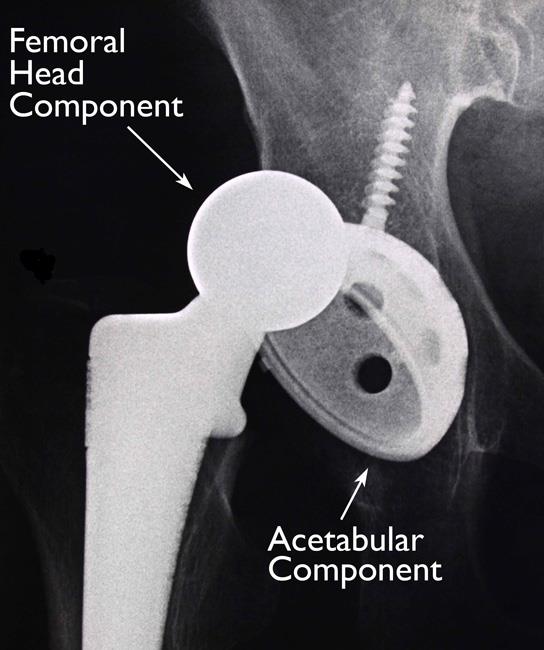
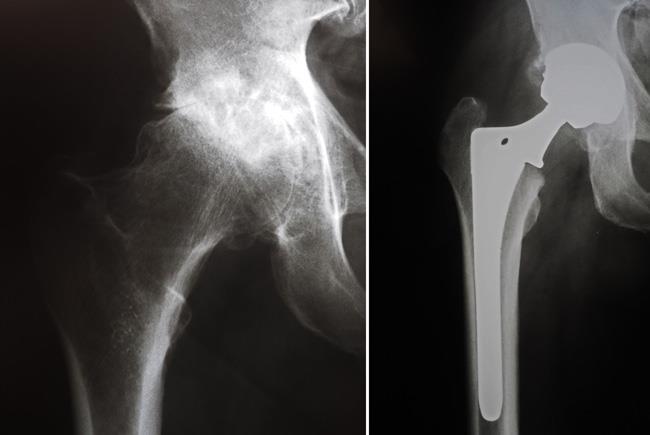
In a total hip replacement (also called total hip arthroplasty), the damaged bone and cartilage is removed and replaced with prosthetic components.
- The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur. The femoral stem may be either cemented or "press fit" into the bone.
- A metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
- The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place.
- A plastic, ceramic, or metal spacer (also called a liner) is inserted between the new ball and the socket to allow for a smooth gliding surface.
Is Total Hip Replacement Surgery for You?
The decision to have total hip replacement surgery should be a co-operative one made by you, your family, your primary care doctor, and your orthopaedic surgeon. The process of making this decision typically begins with a referral by your primary care doctor to an orthopaedic surgeon for an initial evaluation.
When Surgery Is Recommended
There are several reasons why your orthopaedic surgeon may recommend total hip replacement surgery. People who benefit from hip replacement surgery often have:
- Hip pain that limits everyday activities, such as walking or bending
- Hip pain that continues while resting, either during the day or at night
- Stiffness in a hip that limits the ability to move or lift the leg
- Inadequate pain relief from anti-inflammatory drugs, physical therapy, or walking supports
Candidates for Surgery
There are no absolute age or weight restrictions for total hip replacements. Learn more: Obesity, Weight Loss, and Joint Replacement
Recommendations for surgery are based on a patient's pain and disability, not age. Most patients who undergo total hip replacement are 50 to 80 years old, but orthopaedic surgeons evaluate patients individually. Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
The Orthopaedic Evaluation
An evaluation with an orthopaedic surgeon consists of several components:
- Medical history. Your orthopaedic surgeon will gather information about your general health and ask questions about the extent of your hip pain and how it affects your ability to perform everyday activities.
- Physical examination. This will assess hip mobility, strength, and alignment.
- X-rays. These images help to determine the extent of damage or deformity in your hip.
- Other tests. Occasionally other tests, such as a magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your hip.
Deciding To Have Total Hip Replacement Surgery
Talk With Your Doctor
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether total hip replacement surgery is the best method to relieve your pain and improve your mobility. Other treatment options — such as medications, physical therapy, or other types of surgery — also may be considered.
In addition, your orthopaedic surgeon will explain the potential risks and complications of total hip replacement surgery, including those related to the surgery itself and those that can occur over time after your surgery.
Never hesitate to ask your doctor questions when you do not understand. The more you know, the better you will be able to manage the changes that total hip replacement surgery will make in your life.
Learn more: Total Joint Replacement: Questions Patients Should Ask Their Surgeons
Realistic Expectations
An important factor in deciding whether to have total hip replacement surgery is understanding what the procedure can and cannot do.
Most people who undergo total hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living.
With normal use and activity, the material between the head and the socket of every total hip replacement implant begins to wear. Excessive activity or being overweight may speed up this normal wear and cause the total hip replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, or other high-impact sports.
Realistic activities following total hip replacement include unlimited walking, swimming, golf, driving, hiking, biking, dancing, and other low-impact sports.
With appropriate activity modification, hip replacements can last for many years.
Possible Complications of Surgery
The complication rate following total hip replacement surgery is low. Serious complications, such as joint infection, occur in less than 2% of patients. Major medical complications, such as heart attack or stroke, occur even less frequently. However, chronic illnesses may increase the potential for complications. Although uncommon, when these complications do occur, they can prolong or limit full recovery.
Infection. Infection may occur superficially in the wound or deep around the prosthesis. It may happen within days or weeks of surgery. It may even occur years later.
Minor infections of the wound are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis. Any infection in your body can spread to your joint replacement.
Blood clots. Blood clots in the leg veins or pelvis are one of the most common complications of hip replacement surgery. These clots can be life-threatening if they break free and travel to your lungs. Your orthopaedic surgeon will outline a prevention program, which may include:
- Blood thinners (medications that thin the blood)
- Support stockings
- Inflatable leg coverings
- Ankle pump exercises
- Early mobilization
Learn more: Preventing Blood Clots After Orthopaedic Surgery
Leg-length inequality. Sometimes after a hip replacement, one leg may feel longer or shorter than the other. Your orthopaedic surgeon will make every effort to make your leg lengths even but may lengthen or shorten your leg slightly to maximize the stability and biomechanics of the hip. Some patients may feel more comfortable with a shoe lift after surgery.
Dislocation. This occurs when the ball comes out of the socket. The risk for dislocation is greatest in the first few months after surgery while the tissues are healing. However, dislocation is uncommon.
If the ball does come out of the socket, a closed reduction usually can put it back into place without the need for more surgery. In situations in which the hip continues to dislocate, further surgery may be necessary.
Loosening and implant wear. Over a period of years, the hip prosthesis may wear out or loosen. This is most often due to everyday activity. It can also result from a biologic thinning of the bone called osteolysis. If loosening is painful, a second surgery called a revision may be necessary.
Other complications. Nerve and blood vessel injury, bleeding, fracture, and stiffness can occur. A small number of patients continue to experience pain after surgery.
Preparing for Surgery
Medical Evaluation
If you decide to have total hip replacement surgery, your orthopaedic surgeon may ask you to have a complete physical examination by your primary care doctor before your surgical procedure. This is needed to make sure you are healthy enough to have the surgery and complete the recovery process.
Patients with chronic medical conditions, like heart disease or kidney disease, may also need to be evaluated by a specialist, such as a cardiologist or nephrologist, before the surgery.
Tests
Several tests, such as blood and urine samples, an electrocardiogram (EKG), and chest X-rays, may be needed to help plan your surgery.
Preparing Your Skin
Tell your doctor about any skin irritations on the limb that is being operated on, such as cuts, scratches, abrasions, rashes, or bug bites. Any break in skin integrity (the health of the skin) can increase your risk of infection, and if you have an infection, your surgery will be cancelled.
Medications
Tell your orthopaedic surgeon about the medications you are taking. They or your primary care doctor will advise you which medications you should stop taking and which you can continue to take before surgery.
Weight Loss
If you are overweight, your doctor may ask you to lose some weight before surgery to minimize the stress on your new hip and possibly decrease the risks of surgery. Learn more: Obesity, Weight Loss, and Joint Replacement Surgery
Dental Evaluation
Although infections after total hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, major dental procedures (such as tooth extractions and periodontal work) should be completed before your total hip replacement surgery.
For dental procedures after your total hip replacement, talk to your surgeon about whether you need to take preventive antibiotics. And see the suggested amount of time you may need to allow between a dental procedure and a total hip replacement.
In addition, routine cleaning of your teeth should be delayed for several weeks after surgery.
Learn more: Joint Replacement Infection
Urinary Evaluation
Individuals with a history of recent or frequent urinary infections should have a urological evaluation before surgery.
Older men with prostate disease should consider completing required treatment before having total hip replacement surgery.
Social Planning
Although you will be able to walk with a cane, crutches, or a walker soon after surgery, you may need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry.
If you live alone, a social worker or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended care facility during your recovery after surgery also may be arranged.
Learn more: Joint Replacement for Patients With Limited Social or Financial Resources
Home Planning
If you are discharged home after surgery, several modifications can make your home easier to navigate during your recovery. The following items may help with daily activities:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and a shower hose
- A dressing stick, a sock aid, and a long-handled shoehorn for putting on and taking off shoes and socks without excessively bending your new hip
- A reacher that will allow you to grab objects without excessive bending of your hips
- Firm pillows for your chairs, sofas, and car that enable you to sit with your knees lower than your hips
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
- A temporary living space on the same floor, if possible, because walking up and down stairs will be more difficult during your early recovery
Get more tips on preparing your home for your total hip replacement in this infographic (click on image for full infographic).
Your Surgery
You will either be admitted to the hospital on the day of your surgery, or you will go home the same day (this is known as same-day surgery). The plan to either be admitted for at least one night or go home the same day should be discussed with your surgeon before the day of your operation.
Learn more about same-day surgery: Outpatient Total Joint Replacement
Anesthesia
Upon arrival at the hospital or surgery center, you will be evaluated by a member of the anesthesia team. The most common types of anesthesia are:
- General anesthesia (you are put to sleep)
- Spinal, epidural, or regional nerve block anesthesia (you are awake, but your body is numb from the waist down)
The anesthesia team, with your input, will determine which type of anesthesia will be best for you.
Implant Components
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components:
- The ball component (made of highly polished strong metal or ceramic material)
- The socket component (a durable cup of plastic, ceramic, or metal, which may have an outer metal shell)
The prosthetic components may be "press fit" into the bone to allow your bone to grow onto the components, or they may be cemented into place. The decision to press fit or to cement the components is based on several factors, such as the quality and strength of your bone. A combination of a cemented stem and a non-cemented socket may also be used.
Your orthopaedic surgeon will choose the type of prosthesis that best meets your needs.
Procedure
The surgical procedure usually takes 1 to 2 hours. Your orthopaedic surgeon will remove the damaged cartilage and bone and then position new metal, plastic, or ceramic implants to restore the alignment and function of your hip.
After surgery, you will be moved to the recovery room, where you will remain for several hours while your recovery from anesthesia is monitored.
After you wake up, you will either be taken to your hospital room or discharged to home.
Recovery
The success of your surgery will depend largely on how well you follow your orthopaedic surgeon's instructions at home during the first few weeks after surgery (if you are discharged home; if you are discharged to an acute rehabilitation unit or skilled nursing facility, staff there will oversee your post-surgery care).
Pain Management
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including:
- Opioids
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Acetaminophen
- Local anesthetics
Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are narcotics and can be addictive. Opioid dependency and overdose have become critical public health issues in the U.S. It is important to use opioids only as directed by your doctor and to stop taking them as soon as your pain begins to improve. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Wound Care
You may have stitches or staples running along your wound or a suture beneath your skin. The stitches or staples will be removed approximately 2 weeks after surgery.
Avoid getting the wound wet until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Also, be sure to drink plenty of fluids.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within 3 to 6 weeks following surgery. Some discomfort with activity and at night is common for several weeks.
Your activity program should include:
- A graduated walking program — initially in your home and later outside — to slowly increase your mobility.
- Resuming other normal household activities, such as sitting, standing, and climbing stairs.
- Specific exercises several times a day to restore movement and strengthen your hip. You probably will be able to perform the exercises without help, but you may have a physical therapist help you at home or in a therapy center the first few weeks after surgery
Avoiding Problems After Surgery
Recognizing the Signs of a Blood Clot
Follow your orthopaedic surgeon's instructions carefully to reduce the risk of blood clots developing during the first several weeks of your recovery. They may recommend that you continue taking the blood thinning medication you started in the hospital. Tell your doctor immediately if you develop any of the following warning signs.
Warning signs of blood clots. The warning signs of possible blood clot in your leg include:
- Pain in your calf and leg that is unrelated to your incision
- Tenderness or redness of your calf
- New or increasing swelling of your thigh, calf, ankle, or foot
Warning signs of pulmonary embolism. The warning signs that a blood clot has traveled to your lung include:
- Sudden shortness of breath
- Sudden onset of chest pain
- Localized chest pain with coughing
Preventing Infection
A common cause of infection following hip replacement surgery is bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections.
Following surgery, patients with certain risk factors may need to take antibiotics before having dental work, including dental cleanings, or before any surgical procedure that could allow bacteria to enter the bloodstream. Your orthopaedic surgeon will discuss with you whether you need to take preventive antibiotics before dental procedures.
Warning signs of infection. Notify your doctor immediately if you develop any of the following signs of a possible hip replacement infection:
- Persistent fever (higher than 100°F orally)
- Chills
- Increasing redness, tenderness, or swelling of the hip wound
- Drainage from the hip wound
- Increasing hip pain with both activity and rest
Avoiding Falls
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery. Stairs are a particular hazard until your hip is strong and mobile. You should use a cane, crutches, a walker, or handrails or have someone help you until you improve your balance, flexibility, and strength.
Your orthopaedic surgeon and physical therapist will help you decide which assistive aides will be required following surgery, and when those aides can safely be discontinued.
Other Precautions
To ensure proper recovery and prevent dislocation of the prosthesis, you may be asked to take special precautions when sitting, bending, or sleeping — usually for the first 6 weeks after surgery. You may also need to follow precautious during sexual activity. The precautions will vary from patient to patient, depending on the surgical approach your surgeon used to perform your hip replacement.
Your surgeon and physical therapist will provide you with any specific precautions you should follow.
Outcomes
How Your New Hip Is Different
- You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending. These differences often lessen with time, and most patients find these are minor compared with the pain and limited function they experienced prior to surgery.
- Your new hip may activate metal detectors required for security in airports and some buildings. Tell the security agent about your hip replacement if the alarm is activated.
Protecting Your Total Hip Replacement
There are many things you can do to protect your hip replacement and extend the life of your hip implant.
- Participate in a regular light exercise program to maintain proper strength and mobility of your new hip.
- Take special care to avoid falls and injuries. If you break a bone in your leg, you may require more surgery.
- Make sure your dentist knows that you have a hip replacement. Talk with your orthopaedic surgeon about whether you need to take antibiotics prior to dental procedures.
- See your orthopaedic surgeon periodically for routine follow-up examinations and X-rays, even if your total hip replacement seems to be doing fine.
- If you want to resume sexual activity, talk to your surgeon about when it is safe to do so and whether there are any precautions you should take. Learn more: Sexual Activity After Hip Replacement
Last Reviewed
February 2024
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.