Diseases & Conditions
Quadriceps Tendon Tear
Tendons are strong bands of tissue that attach muscles to bones. The quadriceps tendon is the most important tendon involved in straightening the knee from a bent position.
Small tears of this tendon cause pain or make it difficult to walk and participate in other daily activities. A complete tear of the quadriceps tendon is a disabling injury. It almost always requires surgery, followed by physical therapy to regain full knee motion and function.
Quadriceps tendon tears are not common. They most often occur among middle-aged people who play running or jumping sports.
Anatomy
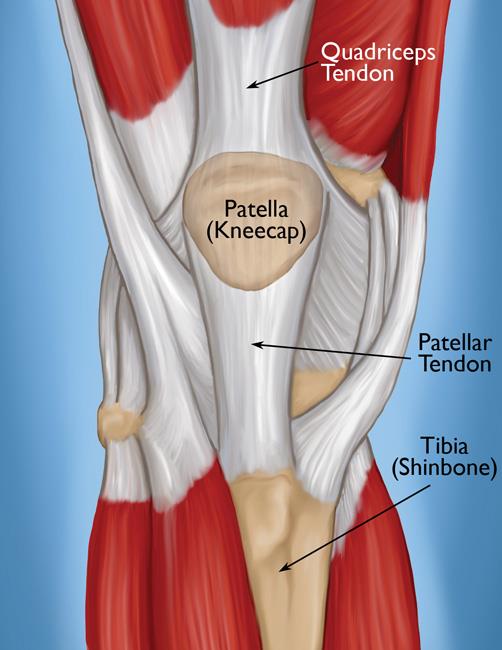
The four quadriceps muscles meet just above the kneecap (patella) to form the quadriceps tendon. The quadriceps tendon attaches the quadriceps muscles to the patella. The patella is attached to the shinbone (tibia) by the patellar tendon. Working together, the quadriceps muscles, quadriceps tendon, and patellar tendon form a pulley mechanism to straighten the knee.
Description
Quadriceps tendon tears can be either partial or complete.
Partial tears. Many tears do not completely disrupt the tendon. This is similar to a rope stretched so far that some of the fibers are frayed, but the rope is still in one piece.
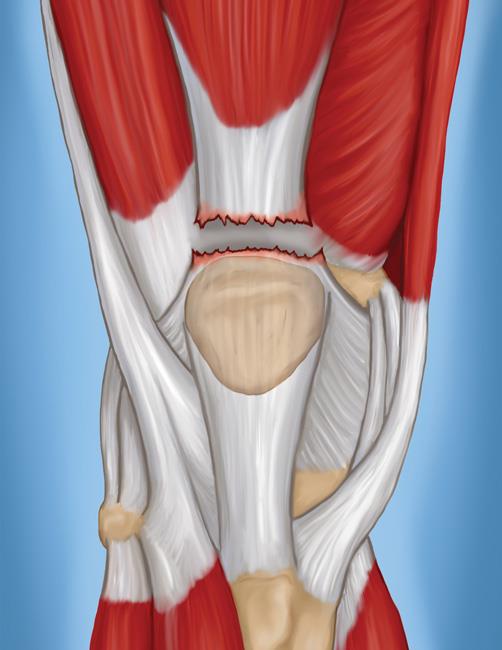
Complete tears. A complete tear will split the soft tissue into two pieces, or the tendon will completely separate from the bone.
When the quadriceps tendon completely tears, the muscle is no longer anchored to the kneecap. Without this attachment, the knee cannot straighten when the quadriceps muscles contract. Patients may experience significant swelling or bruising, or they may notice a divot or gap if they feel the area above the kneecap.
Cause
Injury
A quadriceps tear often occurs when there is a heavy load on the leg with the foot planted and the knee partially bent. Think of an awkward landing from a jump while playing basketball. The force of the landing is too much for the tendon and it tears.
Tears can also be caused by falls, direct force to the front of the knee, and lacerations (cuts).
Tendon Weakness
A weakened quadriceps tendon is more likely to tear. Several things can lead to tendon weakness.
Tendinitis. Inflammation of the quadriceps tendon, called quadriceps tendinitis, weakens the tendon. It may also cause small tears. Quadriceps tendinitis is most common in people who run and participate in sports that involve jumping.
Chronic disease. Weakened tendons can also be caused by diseases that disrupt blood supply. Chronic diseases which may weaken the tendon include:
- Chronic renal (kidney) failure
- Other conditions associated with renal dialysis
- Hyperparathyroidism
- Gout
- Leukemia
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Diabetes mellitus
- Infection
- Metabolic disease
Steroid use. Using corticosteroids has been linked to increased muscle and tendon weakness.
Fluoroquinolones. This special type of antibiotic has been associated with quadriceps tendon tears.
Immobilization. When you are off your feet for a prolonged period of time, the muscles and tendons supporting your knees lose strength and flexibility.
Symptoms
When a quadriceps tendon tears, there is often a tearing or popping sensation. Pain and swelling typically follow, and you may not be able to straighten your knee. Additional symptoms include:
- An indentation at the top of your kneecap where the tendon tore
- Bruising
- Tenderness
- Cramping
- Your kneecap may sag or droop because the tendon is torn
- Difficulty walking due to the knee buckling or giving way
Doctor Examination
Medical History and Physical Examination
Your doctor will discuss your general health and the symptoms you are experiencing. They will also ask you about your medical history. Questions you might be asked include:
- Have you had a previous injury to the front of your knee?
- Have you ever injured a quadriceps muscle?
- Do you have quadriceps tendinitis?
- Do you have any medical conditions that might predispose you to a quadriceps injury?
After discussing your symptoms and medical history, your doctor will conduct a thorough examination of your knee. To determine the exact cause of your symptoms, your doctor will test how well you can extend, or straighten, your knee. While this part of the examination can be painful, it is important to identify a quadriceps tendon tear.
Imaging Tests
To confirm the diagnosis, your doctor may order some imaging tests, such as an X-ray or magnetic resonance imaging (MRI) scan.
X-rays. The kneecap moves out of place when the quadriceps tendon tears. This is often very obvious on a side view X-ray of the knee. Complete tears can often be identified with these X-rays alone.
Magnetic resonance imaging (MRI). An MRI scan creates better images of soft tissues, like the quadriceps tendon, than an X-ray. An MRI is not typically necessary after this injury, as the physical examination is usually telling. However, an MRI can show the amount of tendon torn and the location of the tear if this information is needed. Sometimes, an MRI is required to rule out a different injury that has similar symptoms or to distinguish a partial tear from a complete tear.
Treatment
Your doctor will consider several things when planning your treatment, including:
- The type and size of your tear
- Your activity level
- Your age
Nonsurgical Treatment
Most small, partial tears respond well to nonsurgical treatment.
Immobilization. Your doctor may recommend you wear a knee immobilizer or brace. This will keep your knee straight to help it heal. You will most likely need crutches to help you avoid putting all of your weight on your leg. You can expect to be in a knee immobilizer or brace for 3 to 6 weeks.
Physical therapy. Once the initial pain and swelling has settled down, you can begin physical therapy. Specific exercises can restore the strength and range of motion in your leg.
Your therapist will gradually add exercises to your program. Straight leg raises to strengthen your quadriceps are often central to a physical therapy plan. As time goes on, your doctor or therapist will unlock your brace. This will allow you to move more freely with a greater range of motion. You will be prescribed more strengthening exercises as you heal.
Your doctor will discuss with you when it is safe to return to sports or other physical activity.
Surgical Treatment
Most people with complete tears will require surgery to repair the torn tendon. Your doctor may recommend surgery if you have a large partial tear or a partial tear associated with tendon degeneration. This will likely depend upon your age, your activities, and your previous level of function.
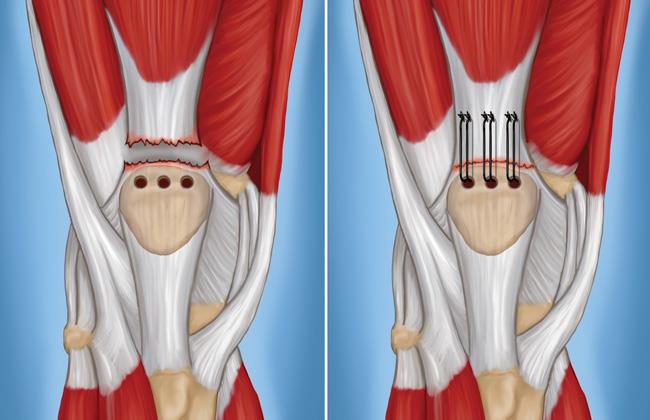
During surgical repair, the surgeon reattaches the torn tendon to the top of the kneecap. People who require surgery do better if the repair is performed soon after the injury. Early repair may prevent the tendon from scarring and tightening into a shortened position.
Hospital stay. Most of the repair procedures are performed on an outpatient basis. Though rare, some people with medical co-morbidities may need to stay in the hospital after their surgery.
The surgery may be performed with regional (spinal) anesthetic, which numbs your lower body, or with a general anesthetic that will put you to sleep.
Procedure. To reattach the tendon, the surgeon places sutures in the tendon and threads the sutures through drill holes in the kneecap. The sutures are carefully tied at the bottom of the kneecap to get the right tension in the tendon. This also ensures that the position of the kneecap closely matches that of your uninjured kneecap.
Alternate Technique. Surgeons may alternatively use suture anchors to reattach the tendon to the bone. With this technique, the surgeon attaches the tendon to the bone using small metal implants called suture anchors. Using these anchors means that the surgeon does not have to drill holes in the kneecap.
Considerations. To provide extra protection to the repair, some surgeons use sutures or cables to help hold the kneecap in position while the tendon heals. If your surgeon does this, the wires or cables may need to be removed during a later, scheduled operation.
Your surgeon will discuss your need for this extra protection before your quadriceps tendon repair surgery. Sometimes, surgeons make this decision for additional protection during surgery, when they see that the tendon shows more damage than expected, or that the tear is more extensive.
If your tendon has shortened too much before surgery, it will be hard to reattach it to your kneecap. Your surgeon may need to add tissue graft to lengthen the tendon. This sometimes involves using donated tissue (allograft).
Tendons often shorten if more than a month has passed since your injury. Severe damage from the injury or underlying disease can also make the tendon too short. Your surgeon will discuss this additional procedure with you prior to surgery.
Complications. The most common complications of quadriceps tendon repair include weakness and loss of knee motion. It is also possible to re-rupture the tendon after it has been repaired. In addition, the position of your kneecap may be different after the procedure.
As with any surgery, other possible complications include infection, wound breakdown, a blood clot, or complications from anesthesia.
After surgery you will require some type of pain management, including ice and medications. About 2 weeks after surgery, your surgeon will remove your skin sutures or staples. This is done in the surgeon's office.
Recovery
- Most likely, your repair will be protected with a knee immobilizer or a long leg cast. You may be allowed to put your weight on your leg with the use of a brace and crutches (or a walker).
- Over time, your doctor or therapist will unlock your brace and allow knee flexion in a step-wise fashion. This will enable you to move more freely with a greater range of motion. Strengthening exercises will then be added to your rehabilitation plan.
- In some cases, your doctor will prescribe an immediate motion protocol (treatment plan). This is a more aggressive approach and not appropriate for all patients. Most surgeons protect motion early on after surgery.
Your doctor and physical therapist will customize a rehabilitation plan for you. How long you need therapy and which exercises your treatment team prescribes will be based on the type of tear you have, your surgical repair, your medical condition, and your needs.
Complete recovery takes at least 4 months. Most repairs are nearly healed in 6 months. Many patients report that they required 12 months before they reached all their goals.
Outcomes
Most people are able to return to their previous occupations and activities after recovering from a quadriceps tendon tear. Slightly over half of people have thigh weakness and soreness at the site of the tear. People who require surgery do better if the repair is performed early after the injury.
If you are a competitive athlete, your surgeon will do very thorough assessment before giving a go-ahead to return to your sport. Your surgeon will compare your leg strength using some functional knee testing (like hopping). The goal is for your injured leg to be at least 85-90% as strong as your uninjured leg. In addition to leg strength, your surgeon will assess your leg's endurance, your balance, and if you have any swelling.
Last Reviewed
October 2021
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.